GM CASE 9
GM case - 9
6 th August 2023
37 year male came to opd with a chief complaint of shortness of breath, decreased urine output,pedel edema, abdominal distension,facial puffiness since 8 days .
Case scenario:
My self Anu Bandlagudem of 3rd BDS .This is an online E log book to discuss our patients de- identified health data shared after taking her guardian's signed informed consent.Here we discuss our individual patients problem through series'of inputs from available global online community of experts with aim to solve those patients clinical problems with collective current best evidence based inputs.
I have been given this case to slove in an attempt to understand the topic of patient clinical data analysis to develop my competency in reading and comprehending clinical data including history, findings, investigations, diagnosis and treatment plan.
Chief complaint:
Shortness of breath
Pedel edema
Decreased urine output
Facial puffiness
Abdominal distension
All since 8 days.
HISTORY OF PRESENT ILLNESS:
Patient is apparently asymptomatic 8 days ago then he developed SOB which is sudden in onset and got aggregated on walking and supine position and relieved on sleeping in lateral positions ( more comfortable in right position ) associated with PND ( paraxysmal nocturnal dyspnea)
and not associated with chest pain with no cough palpations ,, decreased urine output which is drops drops and then he developed abdominal distension after few hours,, pedel edema pitting type till ankle length before he said it was till knee and has pigmentation on limb near lateral malleoli,,.
HISTORY OF PAST ILLNESS:
10 years back had accident and had spinal surgery lost sensation below ankle due to surgery.
5 year back thorn pick leg got infected and right leg got amputated .
6 months back similar complaints of sob
Chest scan Medication done .
12 days back fever with pus discharge near the scrotum region too took medication and got reduced
Since 1 week ko pass of stool
No diabetes mellitus asthama TB hypertension CVA CAD
Epilepsy 15 yrs back
PERSONAL HISTORY:
Patient is conscious coherent coorperative
He is married and have 2 children and he used to do agriculture and an auto driver .
Diet -Mixed
Loss of appetite - yes
Bowel and bladder - decreased
Sleep - okay
Addictions-gutka -from 15 yrs back stopped 10 yrs back
Alcohol - 250 ml occasionally but stopped 1 yr back
Cigarette - 1 packet/ day he started at age of 18 stopped 1 year back
FAMILY HISTORY:
No similar complaints
GENERAL EXAMINATION:
Pallor-no
Icterus-no
Cyanosis-no
Clubbing - no
Lymphadenopathy-no
Edema - yes
No raised jvp
VITALS
Temp - afebrile
Bp - 140/80 mmHg
PR - 60bpm
Respiratory rate - 25 cpm
Systemic examination
Respiratory system examination
INSPECTION:
•Chest is bilaterally symmetrical
Trachea – midline in position.0
Apical Impulse is not appreciated
Chest is moving normally with respiration.
No dilated veins, scars, sinuses.
PALPATION:
•Trachea – midline in position.
Apical impulse is felt on the left 5th intercoastal space.
Chest is moving equally on respiration on both sides
Tactile Vocal fremitus - appreciated
PERCUSSION:
The following areas were percussed on either sides-
Supraclavicular-resonant
Infraclavicular- resonant
Mammary- resonant
Axillary- resonant
Infraaxillary- resonant
Suprascapular- resonant
Infrascapular- resonant
interscapular - resonant.
AUSCULTATION:
•Normal vesicular breath sounds heard.
• crepts present at right basal region
Abdominal examination
Distended
Abdominal rigidity present.
Tenderness present in epigastric region.
No fluid thrill
No shifting dullness
Bowel sounds reduced 3 to 4 / min
CVS examination
S1,S2 heard, no murmurs
PROVISIONAL DIAGNOSIS:
Anascarca
Chronic kidney disease
INVESTIGATION
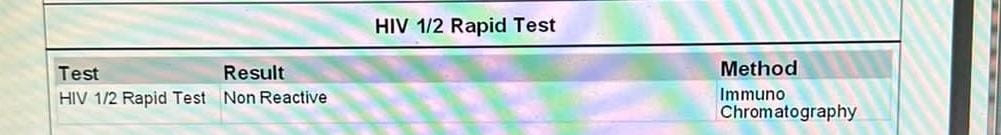
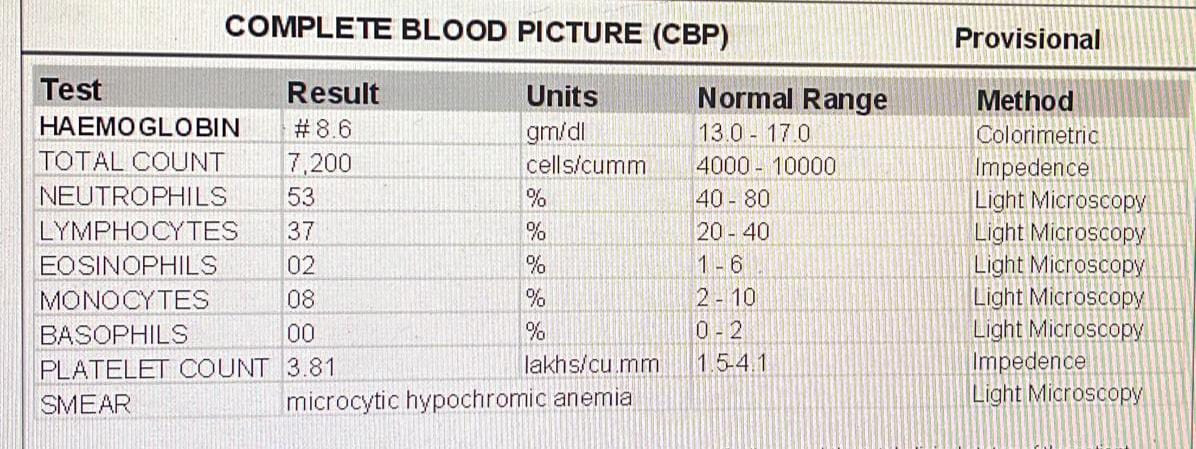
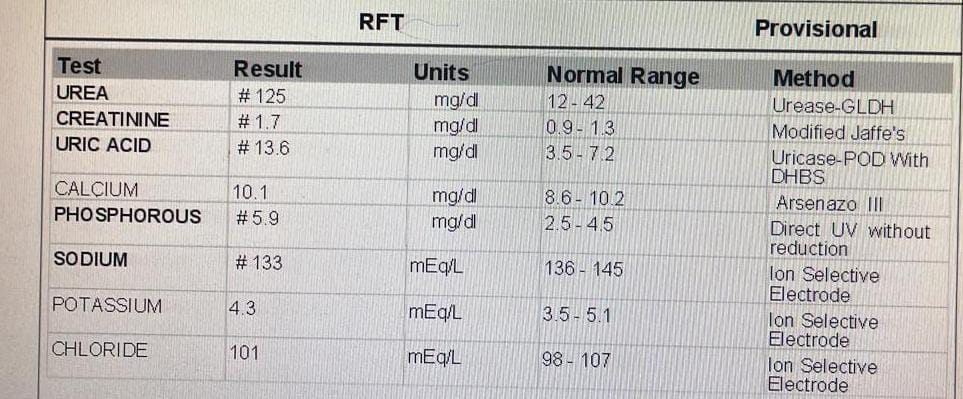
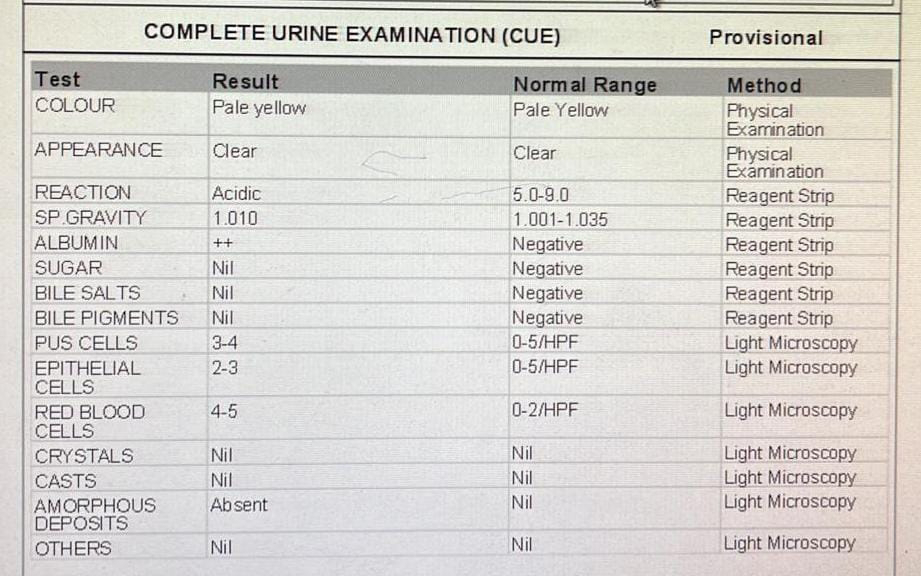
On 28/7/23
ECG ON 29 / 7
6 August 2023
Heart failure
Chronic renal disease
TREATMENT
1.IVF NS @UO + 30 ML/ HOUR
2.INJ. LASIX 40 MG IV/TID( IF SBP MORE THAN 110 MM OF HG)
3.INTERMITTENT CPAP
4.PROTEIN POWDER 2 SCOOPS IN 100 ML MILK OR WATER
5.TAB. OROFER-XT PO/OD
6.TAB.SHELCAL -CT PO/OD
7.TAB. NICARDIA 10 MG PO/TID
Questions :
How can we say patient is a heart failure becoz normal S 1 2 heard with no murmurs with no chest x ray or any investigation?? ( We can tell CKD due to decreased urine output pedel edema and sob ) hw heart failure????