GM case- 7
GM Case 7
18 July 2023
30 year male patient came to opd with a complaints of Vomitings loose stools Shortness of breath since 7 days.
Case scenario:
My self Anu Bandlagudem of 3rd BDS .This is an online E log book to discuss our patients de- identified health data shared after taking her guardian's signed informed consent.Here we discuss our individual patients problem through series'of inputs from available global online community of experts with aim to solve those patients clinical problems with collective current best evidence based inputs.
I have been given this case to slove in an attempt to understand the topic of patient clinical data analysis to develop my competency in reading and comprehending clinical data including history, findings, investigations, diagnosis and treatment plan.
CHIEF COMPLAINT :
Vomitings since 7 days
Loose stools since 7 days
Shortness of breath since 7 days
HISTORY OF PRESENT ILLNESS :
Patient was apparently asymptomatic 7 days ago then he developed vomitings which are non bilious, non projectile , non blood tinged ,filled food particles 10 episodes started during night and continued till morning; loose stools 2 episodes in the morning time which is watery , non blood tinged , non mucopurulent , not associated with fever , pain abdomen; shortness of breath which is grade 3 which is not associated with chest pain , palpitations,orthopnea,PND.
HISTORY OF PAST ILLNESS:
4 years back patient went to local hospital as he is having with decreased urine output and got test done then got to know he is having Diabetes and used medication 1 st he used insulin mixtard 10 U morning and evening 30 min before lunch and dinner respectively, then he shifted to metformin 500 mg + glipizide 5 mg .
4 yr back he visited local hospital with fatigubility,cough,fever,chest swelling and weakness and no strength to work and got his tests done and diagnosed with tuberculosis and used ATT for 6 months .
8 days went to Gandhi hospital and took IV fluids with inHAI 40U.
Not a known case of Hypertension, asthama ,CAD ,CVA, epilepsy, thyroid disorders.
PERSONAL HISTORY:
Married
Diet -Mixed
Appatite - normal
Sleep - adequate
Bowel and bladder -regular
Addictions- alcohol whiskey 90ml
thrice / day
He will wake up at 6 am and takes 10 U of insulin mixtard before 30 min of breakfast and go to work and come home and haves 10C insulin and dinner and sleep by 9 pm and eat rice for his breakfast Lunch and dinner eats chapati or millets only when his glucose level increases, his weight has been reduced from 62 to 48 kgs
FAMILY HISTORY:
Not a known case of diabetes, Hypertension, asthma, epilepsy,cad, stroke,cancer,Tb.
GENERAL EXAMINATION:
Patient is conscious, coherent,
coorperative.
Moderately built and moderately nourished.
Pallor-no
Icterus-no
Cyanosis- no
Clubbing - no
Edema- no
Lymphadenopathy-no
VITALS:
Temprature - 98.7°F
PR-106bpm
RR-23cpm
BP- 130/70mmhg
GRBS- 130mg/dl
SYSTEMIC EXAMINATION:
GIT:
Inspection:
Shape is scaphoid
Flancks - free
Umbilicus - inverted
Skin - scars are absent
Dilated veins - no
Palpation:
Inspectory findings are confirmed
Superficial -
No local rise in temperature
Deep-
Liver - non tenderand non palpable
Spleen - not palpable and non tender
Percussion:
No fluid thrill ( no shifting dullness)
Liver span - 12 cm
No dull sound heard
Auscultation:
Bowel sounds - 9 / min
RESPIRATORY SYSTEM:
Inspection:
Upper respiratory tract:
Oral hygiene - good
No caries
No halitosis
No nasal septum deviation
No sinus tenderness
Tonsils - no
Lowe respiratory tract:
Chest - symmetrical
No drooping of shoulders
Trachea - midline
No supraclavicular / infraclavicular hollowing
Pectus carinatum- no
Pectus excavaum - no
Kphyphoscoliosis - no
Extra nipple is found on chest region
PALPATION:
Inspectory findings are confirmed
Superficial-
No local rise in temperature
Trachea midline
No drooping of shoulders
Crowding of ribs - no
No dilated veins
Deep -
Chest movements - equal
Apical impulse - 5 th intercoastal space lateral to mid clavicular line
Transverse - 32
Anterior posterior - 14
Thoracic circumference - 60
Semi thorax - 30( right and left )
PERCUSSION:
Clavicular - supra and infra
Mamillary
Axillary and infra axillary
Suprascapular and infrascapular
All resonate sound heard
AUSCULTATION:
Normal vesicular breath sounds heard
12 / min
CARDIOVASCULAR SYSTEM:
INSPECTION:
Bilaterally symmetrical chest present
No scars and sinuses
PALPATION:
Inspectory finding are confirmed
Apex beat normal
AUSCULTATION:
S1 S2 heard .
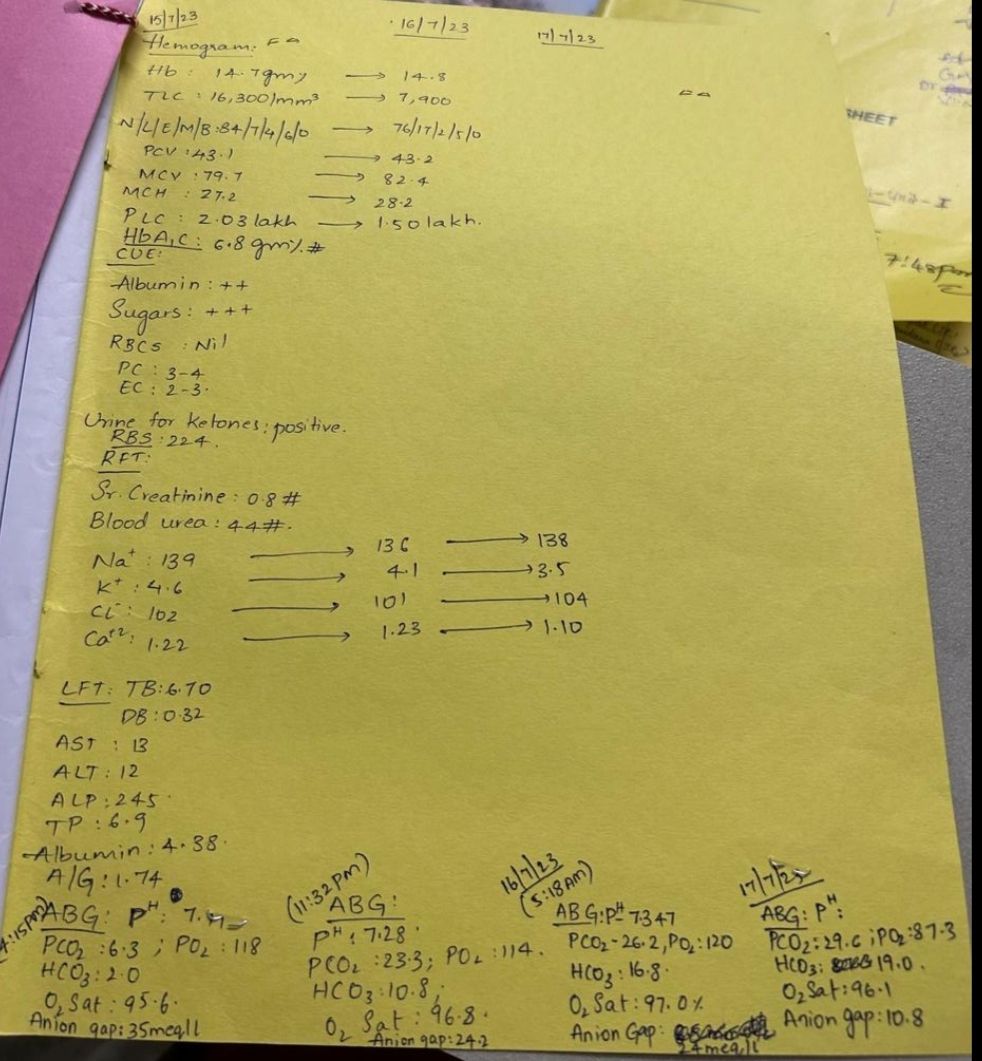
INVESTIGATIONS:
Found ketone bodies in urine , glucose and albumin also positive in urine.
PROVISIONAL DIAGNOSIS:
Diabetic ketoacidosis
.......