GM CASE -8
GM case 8
21 July 2023
A 27 year old female came to opd with a complaints of pain in abdomen .
Case scenario:
My self Anu Bandlagudem of 3rd BDS .This is an online E log book to discuss our patients de- identified health data shared after taking her guardian's signed informed consent.Here we discuss our individual patients problem through series'of inputs from available global online community of experts with aim to solve those patients clinical problems with collective current best evidence based inputs.
I have been given this case to slove in an attempt to understand the topic of patient clinical data analysis to develop my competency in reading and comprehending clinical data including history, findings, investigations, diagnosis and treatment plan.
CHIEF COMPLAINT:
Female patient complaints of pain in abdomen nausea and vomitings since 7 days .
HISTORY OF PRESENT ILLNESS:
Patient was apparently asymptomatic 7 days back then she developed pain in the abdomen that is in the epigastric region which is insidious in onset gradually progressive associated with nausea and vomitings. Pain is burning type with slight radiating towards left and right( left side more than right side ) with are associated with vomitings 3 to 4 episodes per day which is non projectile, non bilious ,with food content, the colour of vomiting is white then changed to yellow colour.
HISTORY OF PAST ILLNESS:
She had a history of eating spicy chicken curry with roti just before the night she experienced pain and then had tea the next day morning which aggregated her pain .she has a habit of eating food with irregular intervals .
Negative history:
No history of cough, chest pain, palpitations,sweating ,shortness of breath,fever, burning micturition.
No history of hypertension, Diabetes mellitus,asthama,TB, epilepsy, thyroid issues.
Had a caesarean (lscs)9 and 5 yrs back .
PERSONAL HISTORY:
Mixed diet
Loss of appetite - no
Bowel and bladder - regular
Sleep - adequate
Urine output - normal
No allergies
No addictions ( tobbacco or alcohol)
FAMILY HISTORY:
not a known case of hypertension diabetes mellitus asthama TB....
But her husband has a history of renal calculus and went on medication andconservation management.
MENSTRUAL HISTORY:
Menarche - 14 yrs of age
2 days of bleeding every month
GENERAL EXAMINATION:
Conscious coherent coorperative
Well built and moderately nourished
Pallor - present
Icterus-no
Cyanosis-no
Clubbing - no
Edema-no
Lymphadenopathy-no
VITALS :
Temp - afebrile
Pulse rate - 65bpm
Respiratory rate - 16 cycles / min
Bp - 100/90 mmHg
Spo2-99%in room temp
SYSTEMIC EXAMINATION:
GASTROINTESTINAL TRACT:
Inspection:
Shape is scaphoid
Flancks - free
Umbilicus - inverted
Skin - scars are absent
Dilated veins - no
Palpation:
Inspectory findings are confirmed
Superficial -
No local rise in temperature
Deep-
Liver - non tenderand non palpable
Spleen - not palpable and non tender
Percussion:
No fluid thrill ( no shifting dullness)
Liver span - 10cm
No dull sound heard
Auscultation:
Bowel sounds - 10/ min
Clavicular - supra and infra
Mamillary
Axillary and infra axillary
Suprascapular and infrascapular
All resonate sound heard
CARDIOVASCULAR SYSTEM:
INSPECTION:
Bilaterally symmetrical chest present
No scars and sinuses
PALPATION:
Inspectory finding are confirmed
Apex beat normal
AUSCULTATION:
S1 S2 heard .Clavicular - supra and infra
Mamillary
Axillary and infra axillary
Suprascapular and infrascapular
All resonate sound heard
RESPIRATORY SYSTEM:
Inspection:
Upper respiratory tract:
Oral hygiene - good
No caries
No halitosis
No nasal septum deviation
No sinus tenderness
Tonsils - no
Lowe respiratory tract:
Chest - symmetrical
No drooping of shoulders
Trachea - midline
No supraclavicular / infraclavicular hollowing
Pectus carinatum- no
Pectus excavaum - no
Kphyphoscoliosis - no
PALPATION:
Inspectory findings are confirmed
Superficial-
No local rise in temperature
Trachea midline
No drooping of shoulders
Crowding of ribs - no
No dilated veins
Deep -
Chest movements - equal
Apical impulse - 5 th intercoastal space lateral to mid clavicular line
Transverse - 50
Anterior posterior - 30
Thoracic circumference - 80
Semi thorax - 40( right and left )
PERCUSSION:
Clavicular - supra and infra
Mamillary
Axillary and infra axillary
Suprascapular and infrascapular
All resonate sound heard
AUSCULTATION:
Normal vesicular breath sounds heard
12 / min
PROVISIONAL DIAGNOSIS:
Gastritis
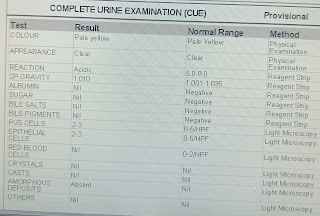
INVESTIGATIONS:
Serum creatinine: 0.8
Blood urea: 14mg/dl
RBS : 84mg/dl
Albumin: 3.71
Serum Na+ :145 mEq/L
Serum K+ : 4.0 mEq/L
Serum Cl- :102 mEq/L
DEFINITIVE DIAGNOSIS:
Gastritis
Renal calculus
Tiny hypercholic foci in gall bladder ( gall stones ).